Cataract Awareness Month
June is Cataract Awareness Month
Cataracts are the leading cause of blindness in the United States, according to Prevent Blindness America, which declared June as Cataract Awareness Month. Cataracts affect more than 24 million Americans 40 and older. More than half of all Americans have cataracts by the time they are 80 years old, but cataracts can also appear in young adults or even newborns. Prevent Blindness America (PBA) estimates that by 2020, 30 million Americans will have cataracts. Unlike many other causes of vision loss, vision loss resulting from cataracts can be managed or significantly restored. There is no better time than Cataract Awareness Month to learn the symptoms and risk factors of cataracts, and to schedule an appointment with your eye care professional.
What Causes Cataracts?
There are several risk factors that may lead to cataracts, including:
- Heredity–family history of cataracts
- Inflammation of the eye
- Certain diseases such as diabetes or metabolic disorders, which can increase your risk of developing cataracts
- Intense heat or long-term exposure to UV rays from the sun
- German measles while pregnant can cause the newborn to be born with cataracts
- Long-term steroid use
- Eye injury, also known as traumatic cataracts
- Hypertension
- Smoking or alcohol use
- High myopia, or nearsightedness
- Medications such as statin medicines used to reduce cholesterol, or hormone replacement therapy
Cataracts may develop in one eye, particularly traumatic cataracts. More often, they develop in both lenses. Like myopia or astigmatism, they don’t always advance in the same way or at the same rate. One eye can have greater vision loss than the other as cataracts develop.
How does Cataracts Affect Vision?
The lens of the eye contains mostly water and protein. The protein in the eye is normally arranged in a way that keeps the lens clear, allowing light to pass through it. Cataracts occur when proteins in the lens of the eye begin to clump up.
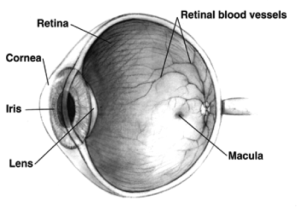
The lens of the eye acts as a camera lens. It focuses light on the retina for clear vision. It also adjusts the eye’s focus, helping us to see things both close and far away.
There are several types of cataracts, and they are categorized by where they form and what causes them.
- A subcapsular cataract forms at the back of the lens. This type is more common in people with diabetes or those taking high doses of steroids. This form of cataract will interfere with reading and reduce your vision in bright light and can cause glare or halos around lights at night.
- A nuclear cataract forms in the nucleus (central zone) of the lens. These cataracts most often occur because of aging. This cataract will turn your lenses brown and interfere with your ability to detect color.
- A cortical cataract forms white, wedge-like opacities that start at the edge of the lens and work their way to the center. They look like wagon spokes and form in the lens cortex. This is the part of the lens that surrounds the central nucleus. These types of cataracts affect your peripheral vision and causes problems with glare.
Since cataracts tend to form over a long period of time, you may not know you have a cataract for years. If left undiagnosed, your vision may eventually acquire a brownish shade. Here, the cataract doesn’t affect your vision. As cataracts progresses, you may lose the ability to identify blues and purples. Your vision will start to dull or blur, and you will develop poor night vision, and halos may appear around lights, headlights, or lamplights. Having to change prescriptions in your eyeglasses or contacts regularly can also be a sign of a developing cataract.

How are Cataracts Detected?
A comprehensive eye exam includes testing for cataracts and other disorders of the eye such as macular degeneration and glaucoma.
You can expect:
- A review of your personal and family health history including any history of eye problems.
- A visual acuity test to determine how well you see at various distances.
- A dilated eye exam, where drops are placed in your eyes to dilate your pupils. Your retinas and optic nerves will be examined for signs of damage and other issues.
- Tonometry will measure the pressure inside the eyes. Numbing drops might be applied for this test.
If your doctor detects signs of a cataract, they might do additional testing to see whether your eyes are sensitive to light or if your peripheral vision (side vision) is affected.
If you are Diagnosed with Cataracts
There are several treatment options available for cataracts, depending on the severity. Your eye care professional will probably recommend new eyeglasses, brighter lighting, anti-glare sunglasses, or magnifying lenses. If these measures prove unsuccessful, the only option left is surgery. Some people can go years before needing surgery.
When the Treatment is Surgery
Traditional cataract surgery typically involves using a blade to remove the clouded lens and replacing it with an artificial one. It is usually only recommended when vision loss interferes with your daily activities, but it can also be recommended if it interferes with the eye care professional’s ability to examine or treat the rest of your eye. Laser cataract surgery provides a level of safety and comfort similar to bladeless LASIK where a femtosecond laser is used to make to make the incision.
Cataract surgery can slightly increase your risk of retinal detachment especially if you have other eye conditions which can also increase your risk. Talk with your eye care professional about the pros and cons of any options you are considering.
That said, cataract surgery is one of the most commonly performed surgeries, and is usually an outpatient procedure. More than 3 million Americans undergo cataract surgery every year, according to PBA. Nearly nine out of ten people who have cataract surgery regain very good vision, between 20/20 and 20/40.
It is important to speak with your doctor about vision issues you might be having, and to make informed decisions about the care and protection of your eyes. Your eye care professional should be able to sit down with you and discuss all your risk factors and help you weigh those against the benefits of the treatment options offered. If you are 65 or older, it’s important to get a complete eye exam every one or two years, even if you have no problems seeing. Schedule your appointment during Cataract Awareness Month and be proactive about your eye health.
Cataract Newsletter
Cataract Surgery Risks and Benefits
Cataract surgery has changed over the past 20 years from large incisions with long recovery times to our current surgery with a 2.4mm incision, self sealing wound, and possible expectations of refractive benefits where glasses are not required for distance nor near. Some of the greatest difficulties with cataract surgery involve managing reasonable expectations.
This letter will review cataract surgery and its risks and benefits. It will focus on the new refractive options that are available because of new lens designs. Lastly, it will review unexpected benefits about glaucoma.
Cataract surgery involves the removal of a cloudy lens from the center of the eye and its replacement with a thin plastic lens that is designed to focus the light on the retina. The normal lens is optically clear but as we age, and occasionally in association trauma or illness, the lens becomes cloudy and discolored. It is no longer able to focus the light but rather causes the light to amplify or scatter in a random manner, what you might describe as glare or blurred vision. If these changes interfere with your daily activities and quality of life, it is reasonable to consider surgery. Your doctor will also consider other factors, beyond the scope of this letter, when considering your cataract.
While cataract surgery is one of the most successful and predictable surgeries, risks are still present. To each patient it remains a major surgery as there is the potential for vision loss and rarely actual loss of the eye from infection, bleeding or retinal detachment.
The excitement of cataract surgery comes from the refinements in instruments that allow a very small self sealing wound and the precise calculation of a monofocal lens implant that minimizes the need for glasses after surgery. Often, the residual refractive error, or need for glasses, is not significant and the patient is content with only reading glasses.
The special lens is also available to treat most astigmatism. These toric lenses are aligned with your eye to treat the moderate corneal irregular curvature that is not treated by a standard lens. The higher level of premium lens implant is a multifocal lens that is designed to minimize the need for distance and near vision glasses. There are multiple brands that utilize different technologies, but the goal is to have some light focused for near and some for far. This may limit contrast sensitivity and can be associated with a glare but for many patients, the benefits far exceed these issues. Not every patient is a candidate for the toric or the multifocal implant and for that reason, Medicare allows an out of pocket charge for the extra evaluation and services. Patients with dry eyes or other surface abnormalities do not tolerate these lenses well, and some consider macular degeneration to be a relative contraindication. Your doctor will take these factors into consideration if you are considering a premium lens implant.
Recent studies have highlighted other benefits of cataract surgery.
 The Ocular Hypertension Treatment Study reported on the benefits of cataract surgery in patients with ocular hypertension in September 2012. The report had a better design and confirmed what other studies had reported, a reduction in postoperative intraocular pressure. There was an average 16.5% reduction in IOP and there was a greater reduction in eyes with the highest preoperative pressure. A lower intraocular pressure limits the potential for glaucoma damage and in some patients may make glaucoma drop therapy no longer necessary. This can be a considerable financial saving given the price of glaucoma medications.
The Ocular Hypertension Treatment Study reported on the benefits of cataract surgery in patients with ocular hypertension in September 2012. The report had a better design and confirmed what other studies had reported, a reduction in postoperative intraocular pressure. There was an average 16.5% reduction in IOP and there was a greater reduction in eyes with the highest preoperative pressure. A lower intraocular pressure limits the potential for glaucoma damage and in some patients may make glaucoma drop therapy no longer necessary. This can be a considerable financial saving given the price of glaucoma medications.
In July 2012, a new study published in The Journal of the American Medical Association examined the incidence of hip fractures in the year after cataract surgery. The study showed 16% fewer hip fractures in the year after surgery. Interestingly, the patients between the ages of 65 and 69 had a slightly higher rate of hip fracture but the patients ages 80 to 84 experienced a 28% reduction in hip fractures compared to those Medicare beneficiaries who did not have cataract surgery.
Other studies have shown benefits in mental health and overall quality of life after cataract surgery. It is a very exciting time in ophthalmology and cataract care. It is amazing to think of the distance we have covered in the last 20 years. While all surgeries carry some risk, there is a lot more to be excited about than feared when you are told, “ You have cataracts and we need to consider surgery to make you see better.”
For more information please visit our Home Page.
Cataract Surgery Risks and Benefits
Cataract Operation Risks and Benefits
This letter will review cataract surgery and its risks and benefits. It will focus on the new refractive options that are available because of new len’s designs. Lastly, it will review unexpected benefits with respect to glaucoma.
While cataract surgery in is one of the most successful and predictable eye surgeries in Savannah, risks are still present. To each patient it remains a major surgery as there is the potential for vision loss and rarely actual loss of the eye from infection, bleeding or retinal detachment.
The excitement of cataracts operations come from the refinements in instruments that allow a very small self sealing wound and the precise calculation of a monofocal lens implant that minimizes the need for glasses after surgery. In many cases, the residual refractive error, or need for glasses, is not significant and the patient is content with only reading glasses.
The special lenses are also available to treat most astigmatism. These toric lenses are aligned with your eye to treat the moderate corneal irregular curvature that is not treated by a standard lens. The higher level of premium lens implant is a multifocal lens that is designed to minimize the need for distance and near vision glass. There are multiple brands that utilize different technologies, but the goal is to have some light focused for near and some for far.
This may limit contrast sensitivity and can be associated with glare but for many patients, the benefits far exceed these issues. Not every patient is a candidate for the toric or the multifocal implant and for that reason; Medicare allows an out of pocket charge for the extra evaluation and services. Patients with dry eyes or other surface abnormalities do not tolerate these lenses well, and some consider macular degeneration to be a relative contraindication. Your doctor will take these factors into consideration if you are considering a premium lens implant.
 Recent studies have highlighted other benefits of cataract surgery
Recent studies have highlighted other benefits of cataract surgery
The Ocular Hypertension Treatment Study reported on the benefits of cataract operation in patients with ocular hypertension in September 2012. The report had a better design and confirmed what other studies had reported, a reduction in postoperative intraocular pressure. There was an average 16.5% reduction in IOP and there was a greater reduction in eyes with the highest preoperative pressure. A lower intraocular pressure limits the potential for glaucoma damage and in some patients may make glaucoma drop therapy no longer necessary. This can be a considerable financial saving given the price of glaucoma medications.
In July 2012, a new study published in The Journal of the American Medical Association examined the incidence of hip fractures in the year after a cataract procedure. The study showed a 16% fewer hip fractures in the year after surgery. Interestingly, the patients between the ages of 65 and 69 had a slightly higher rate of hip fracture but the patients ages 80 to 84 experienced a 28% reduction in hip fractures compared to those Medicare beneficiaries who did not have cataract surgery.
Other studies have shown benefits in mental health and overall quality of life after cataract surgery. It is a very exciting time in ophthalmology and cataracts care. It is amazing to think of the distance we have covered in the last 20 years. While all surgeries carry some risk, there is a lot more to be excited about than feared when you are told, “ You have cataracts and we need to consider a procedure to make you see better.”
Macular Degeneration, Aspirin and Cataract Surgery
 Macular Degeneration Relationship to Daily Aspirin and Cataract Surgery
Macular Degeneration Relationship to Daily Aspirin and Cataract Surgery
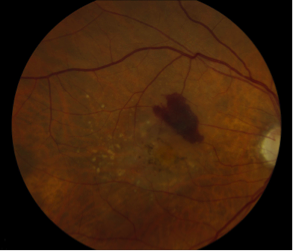
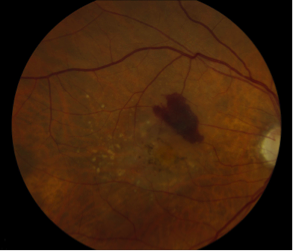
Age related Macular degeneration (AMD) is a leading cause of vision loss. It is a major health issue as our population ages and is eager to maintain independence. Preserving central vision allows us to drive and read our mail. Macular degeneration is referred to as dry or wet based on your physicians clinical findings.
Dry macular degeneration is characterized by a progressive thinning and atrophy of the macular region that results in poor central vision. Patients often describe a slow decline of vision with complaints of worsening contrast vision and the need for better lighting. You can think of it as “thread bare “ areas near the central vision that slowly expand leading to larger zones where there is no retina to receive the focused image. This only involves the central retina, or macula, and patients maintain peripheral vision. There is no bleeding or leakage of fluid into the retina.
Wet Age-Related Macular Degeneration
Wet age related macular degeneration, however, does involve bleeding and leakage of fluid into the central retina. This may occur relatively sudden and seemingly without warning. Common symptoms can include: sudden distortion of images or straight lines, a central gray or dark area, or just blurred vision. Early symptoms can be missed as we rarely check each eye individually and one eye may have problems while the other eye allows normal function. The bleeding and leakage of fluid associated with wet macular degeneration is the result of abnormal new vessels growing in the macular region. These new vessels tend to be fragile and may break and bleed without any action on your part.
As we age and become at risk for vascular events, prophylactic aspirin (ASA) has almost become a standard of care. This attempt to prevent clotting and its associated morbidities are obviously at odds with the goals of our wet macular degeneration patients. Many studies have looked at the association between ASA and wet AMDwith respect to causation and prognosis. It is a complex question as vascular disease is more common in patients with macular degeneration and smoking is an independent risk factor for both conditions.
In January 2012 The European Eye (EUREYE) Study reported on the association of ASA and AMD, as determined by questionnaire, within a group of 4700 patients. There was a variable use of ASA and of AMD severity among the participants and they showed that “frequent aspirin use was associated with early and wet late AMD” and the odds were greater with increasing frequency of ASA use. This cross sectional study did not determine causation but only says there may be a link. Obviously, each patients use of ASA or any other supplement must be evaluated on an individual basis but a practical assessment would be that prevention of stroke or heart attack with ASA use will outweigh any concern of ASA causing macular degeneration. The benefit of a healthy diet in green leafy vegetables and smoking cessation far outweigh any concerns associated with aspirin use.
For those patients with newly diagnosed wet AMD and active bleeding, it is reasonable to discuss a change in anticoagulant therapy for the short term. Drugs like Plavix, Coumadin, Pradaxa, and aspirin can exacerbate the bleeding with wet AMD in the short term. Fortunately, the new injection therapies cause regression of the offending new vessels and thereby dramatically reduce the risk of bleeding after a few injections.
Cataract Operation
Another common association and concern is whether a cataract eye operations cause macular degeneration to advance. There are over 3,000,000 cataract surgeries performed each year in the U.S. and many studies have explored this relationship. In November 2009, The Age-Related Eye Disease Study Report No. 27 reviewed 1939 eyes that had cataract surgery while enrolled in the national trial that evaluated antioxidants and minerals in macular degeneration. Each group showed a gain in vision but there was a declining benefit with more advanced pre-existing AMD. The benefit ranged from a gain of more than 8 letters in the group without AMD to only 2 letters gained in the advance AMD group.
In November 2012 the Australian Cataract Surgery and Age-related Macular Degeneration (CSAMD) study reported on the possible association between cataract surgery and the progression of AMD. This study used a fellow eye comparison so that it only included patients who had cataract surgery in one eye and left the other cataract alone for two years. Cataract operations were performed in 1851 patients and 71% had 36 months of follow up. The study showed no increased risk of early AMD or late AMD. There was a slight increase in retinal pigmentary changes in the operated group but the significance is yet to be determined.
Conclusion
Macular degeneration is a complex disease with many contributing factors including genetics, diet, smoking, and exercise patterns. Each study sheds a little more light on the subject but often leaves us with more questions. We believe it is safe to conclude the following:
- A diet that contains green leafy vegetables and fresh fruits is recommended. Vitamin supplementation with an AREDS approved vitamin is advised for patients with intermediate or advanced macular degeneration in one eye.
- It is reasonable to use aspirin on a daily basis but the patient’s eye care specialist should be aware of use of any anticoagulants for other medical conditions.
- Cataract surgery is safe in patients with macular degeneration but it is reasonable to evaluate with a retinal scan or have a retinal consultation before surgery if there is any doubt about the role of AMD in a patient’s vision loss.
- Tobacco cessation is necessary and cessation counseling should be provided.
LenSx Press Release
Georgia Eye Institute Revolutionizing Cataract Surgery
With Introduction of First Laser Assisted Cataract Surgery in the Greater Savannah Area
SAVANNAH, GA: February 17, 2013 –Ophthalmic surgeons at Georgia Eye Institute are now able to offer patients an all-laser, blade-free method of cataract surgery that is revolutionizing one of the most common procedures performed in medicine today.
Femtosecond laser cataract surgery using the LenSx Laser System offers a reproducible, noninvasive technique to replace the least predictable – and most technically demanding – steps for surgeons during conventional cataract procedures. Cataract removal and lens implantation is one of the most common – and successful medical procedures performed today. Each year, more than two million people in the United States have their vision restored through cataract surgery.
In addition, the laser’s advanced technology makes break-up and removal of the cataract easier and gentler on the patient.
The surgeons of Georgia Eye Institute are among the top 10% surgeons in the United States to offer patients the safety, precision and accuracy of the laser assisted cataract surgery. Georgia Eye Institute is the first practice in the greater Savannah area to give patients access to this advanced laser technology.
Laser assisted cataract surgery makes laser correction of astigmatism now possible with more precise and predictable laser-guided application. In the post-operative recovery period following laser cataract surgery, there is less incidence of swelling and inflammation than with traditional cataract surgery.
According to the latest information from Alcon, Inc. – who manufactures and distributes LenSx lasers – national outcomes continue to be very promising with patients achieving early visual recovery and consistent results. The LenSx laser procedure is surgeon-directed, computer controlled and allows for added precision during surgery. This allows most patients to return to their normal activities sooner.
Each human eye varies according to size, depth, curvature of the cornea and other essential factors. In preparation for cataract surgery, every eye is carefully measured and mapped. The laser uses a combination of highly advanced technologies to capture extremely precise, high-resolution digital images of the eye. “These real-time images, plus the measurements and data they provide, are then used to plan and perform a surgery to customized specifications that were previously unachievable,” notes Dr. Reeves of the Georgia Eye Institute.
Cataract development is simply part of the natural aging process and is quite common in everyone over age 50. Cataracts occur when the natural clear lens of the eye becomes progressively cloudy, causing colors to become less vibrant normal vision to become blurred. The only method to treat a cataract is through surgical removal of the body’s natural lens and implanting an artificial lens.
Cataract surgery has evolved over the years from a procedure with less than certain outcomes, to an advanced no-patch, no-shot, no-stitch, 10-minute procedure with a swift recovery time.
Georgia Eye Institute is one of the region’s most established full-service comprehensive eye care provider. We offer patients convenient access at any one of our 13-area locations and can be reached at 912-354-4800.
