Diabetic Retinopathy FAQs
What is diabetic retinopathy?
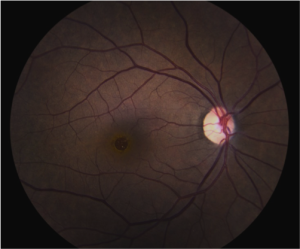
Long-standing diabetic disease (in Type I or Type II diabetics) can lead to changes in the back of the eye that can cause a decrease in vision. Specifically, high blood sugar causes damage to the small blood vessels in the retina (layer at the back of the eye that sense light). This damage leads to multiple changes to the retina, especially to the macula, which is responsible for central vision (Figure 1).
What are the different types?
There are two main types of diabetic retinopathy – “Non proliferative Diabetic Retinopathy” and “Proliferative Diabetic Retinopathy.” Proliferative indicates that new, abnormal blood vessels are growing inside the eye, which can lead to bleeding, retinal detachment, and high pressure (all leading to vision loss). Proliferative disease is more sever, but legal blindness can be caused by changes from non-proliferative disease.

Figure 1 – Normal Macula (the central part of the retina responsible for central vision)
Why do people lose vision from diabetic retinopathy?
Diabetes can lead to vision loss for many reasons, including:
- Swelling in the center part of the vision (Macular edema)
- Loss of blood flow to the center part of the vision (Macular ischemia)
- Bleeding into the central part of the eye (Vitreous hemorrhage)
- Detachment of the back layer of the eye from scar tissue (Retinal detachment)
How is it diagnosed?
The retina can be visualized during a routine eye exam after dilation of the pupil (Figure 3). Optical coherence tomography is a type of non-invasive imaging that allows your physician to view the macula and macular edema (if present) in cross-section (Figures 3 and 4). This is useful for following the disease over time.
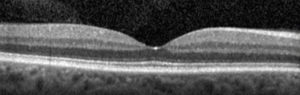
Cross sectional image (Optical Coherence Tomography, or OCT) of a normal macula. The “dip” in the center is the very center part of the vision, or the “fovea.” This is the “20/20? portion of the vision.
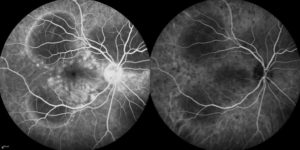
Figure 5. Photograph of the retina (angiogram) that shows loss of blood flow (dark areas).
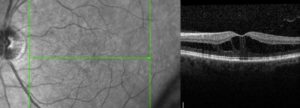
Figure 4. Cross sectional image (OCT) of a macula with diabetic macular edema. Notice the loss of the “dip” and black spaces in the retina. The retina is also thicker because of the swelling. This thickening leads to decreased vision.
How is it treated?
Treatment of diabetic retinopathy depends on the type of disease present. Good blood glucose and blood pressure control are essential in stabilizing disease.
Macular Edema
Edema that affects the center part of the vision is initially treated with medication that is injected into the eye (Figure 6). There are several medications available (Avastin, Lucentis, Eylea, Osurdex implant, steroid). For certain types of edema laser may be used. Laser can be used to destroy leaking blood vessels. A newer technology (micropulse laser) uses non-destructive energy to cause the macula to release factors that cause vessels to stop leaking.
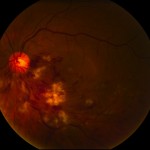
Figure 6. After the surface of the eye is anesthetized (numbed), a small amount of medication is injected into the middle of the eye (vitreous).
Proliferative Diabetic Retinopathy
Proliferative disease (especially if associated with bleeding [vitreous hemorrhage]) is generally treated with laser (panretinal photocoagulation). Laser is used to destroy sick tissue (areas in the back of the eye with loss of blood flow) – this causes abnormal blood vessels to shrink/resolve (Figure 7).
Vitreous Hemorrhage and Traction Retinal Detachment
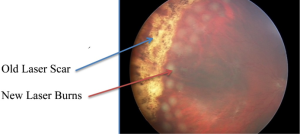
Figure 7. Photo of the retina shows vitreous hemorrhage covering the macula (center of vision) which blurs the vision. Laser scar can be seen peripheral to the blood. This patient required vitrectomy (surgery) to remove the blood.
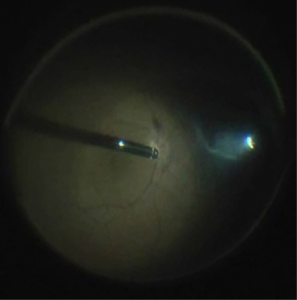
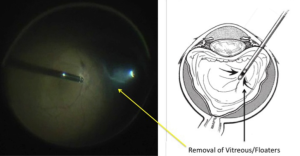
Proliferative disease that is untreated will lead to bleeding and retinal detachment. The blood itself will usually not harm the eye and will often resolve spontaneously. If the blood does not resolve or if there is retinal detachment that treats the macula (center part of the vision), surgery (vitrectomy) is necessary,. This surgery is performed in an operating room. Small instruments are introduced through micro-cannulas. One instrument provides light and the other instruments to remove blood and scar tissue and place additional laser (Figure 8).
When should a diabetic have a complete eye exam?
A type I diabetic should have their eyes examined within 3-5 years after diagnosis and yearly thereafter if no eye disease is found. A type II diabetic should have their eyes examined at the time of diagnosis and yearly thereafter if no eye disease is found. If diabetic retinopathy is present, follow-up and treatment depends on the severity of the disease or any other issues you may have.

Removal of the vitreous from inside the eye using the “vitrector” (left side of picture). A small instrument (right side of picture) provides the light to see inside the eye. This is done under a microscope.
6 Tips to Maintain Healthy Vision
6 Tips You Can Do Right Now to Maintain Healthy Vision
#1 – Wear Sunglasses
You probably know the sun can damage your skin… but did you realize the risk the sun poses on the health of your eyes? While sunglasses are a great aesthetic accessory, protection from UV Rays is ultimately what they’re used for.
Be careful to avoid these harmful side effects from the sun:
- Cataracts, which is when the lens of the eyes becomes cloudy, resulting in blurred vision. Approximately 20% of all cases are a result of UV exposure.
- Macular Degeneration happens when the retina is damaged and destroys central vision. This is the leading cause of blindness.
- Pterygium is a growth of tissue on the white part of the surface of your eye that affects the curve of your eyeball. The result is astigmatism.
When purchasing sunglasses look for something that blocks almost 100% of UVB and UVA radiation.
#2 – Quit Smoking
Did you know smoking can be harmful to your eyes? Sight -related problems are rarely discussed, so here are a few reasons that might help you kick the habit:
- Studies show that smokers are at three times the risk for developing AMD, and female smokers aged 80 plus are over 5.5 times likely to acquire AMD than those that don’t smoke and are the same age.
- Smoking doubles the risk of diabetes. Smoking is also a risk factor for progression of diabetic retinopathy, and hypertension.
- Smokers show higher rates of blindness and other issues in old age.
#3 – Annual Eye Exams Are Necessary
Recent studies have found that 25% of adults have not had their eyes checked in the last two years. Studies also show that 25% of all people are unaware that a simple eye exam can prevent blindness. If you’ve had laser vision surgery or are naturally blessed with good vision, it is still recommended that you have regular eye exams, preferably annually (after age 40).
“Vision tests” are not the same as having a complete eye exam. A thorough eye exam performed by an optometrist or ophthalmologist can detect potentially harmful diseases, vision disorders, and issues with the muscles in your eyes. If things begin to look blurry or you have trouble seeing objects far or near, this is an indication that you should have your eyes checked.
 #4 – Healthy Eating for Healthy Vision
#4 – Healthy Eating for Healthy Vision
There is a strong connection between food and one’s overall health. It has become apparent that having a healthy diet rich in vitamins and minerals provides long-term protection for your vision. Physicians tell us, “One of the best things you can do for your eyes is to eat a balanced diet high in fruits and vegetables, but also low in saturated fats and sugar.
#6 – Ensure the health of your Eyes by Washing Your Hands
The number of times you wash your hands daily can prevent the spread of infectious diseases, according to the Centers for Disease Control. By washing your hands frequently, you prevent the collection of dirt and germs that may be easily transferred to the eyes. This is caused by we touch this area subconsciously throughout the day. Not only will it reduce the chances of getting sick, it also helps control the spread of bacteria and viruses that are responsible for causing as-conjunctivitis (pinkeye) as well as corneal ulcers.
A great habit to practice is washing your hands before you eat or prepare food, before you treat injuries, before using any type of dispensing machine, and before you take out or put in contact lenses. An important instance where washing your hands should be your number one priority is before you get something in your eye or eyelash.
Some quick facts to digest when it comes to the protection of your eyes via washing your hands:
- Half of all people fail to wash their hands after sneezing or coughing.
- Over half of all men and almost one fourth of women doesn’t wash their hands after using restroom facilities.
- Over one third of all people don’t think it is necessary to wash their hands before a meal.
- Left-handed people tend to wash their right hand more thoroughly than they’re left and conversely for right handed people.
We hope these tips help you in your quest for top-notch vision! For more information please visit our Homepage.
Flashers, Floaters and Retinal Detachment
What are flashers and floaters? What causes them?
The center of the eye is filled with a clear gel called vitreous. When we are born, the vitreous in both eyes is completely clear and stuck down everywhere to the inside surface of the eye (including the retina). As we get older the gel clumps together, these cast shadows on the retina (light sending part of the eye) causing the occasional floaters we see.
After several decades (usually after age 50) the gel liquefies and starts to separate from the back of the eye. This is called posterior vitreous separation, or detachment. When this occurs a larger floater can be seen. People sometimes describe this as a circle, a cobweb, a spider, etc. (Figure 1).
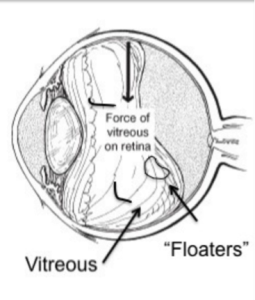 As the separation progresses (usually over 4-6 weeks) the gel can tug on the retina (back of the eye). This causes flashes of lights. Though the flashes do not cause damage, a flash could indicated that the gel is pulling especially hard increasing risk of a tear in the retina.
As the separation progresses (usually over 4-6 weeks) the gel can tug on the retina (back of the eye). This causes flashes of lights. Though the flashes do not cause damage, a flash could indicated that the gel is pulling especially hard increasing risk of a tear in the retina.
The appearance of flashes and floaters may be alarming, especially if they develop suddenly. You should contact your eye doctor right away if you suddenly develop new flashes or floaters.
Are floaters ever serious?
The retina can tear if the shrinking vitreous gel pulls away from the wall of the eye. This sometimes causes a small amount of bleeding in the eye that may appear as new floaters. A torn retina (Figure 2) is always a problem, since it can lead to a retinal detachment. You should call your eye doctor as soon as possible if:
- Even one new floater appears suddenly
- Lots of “pepper spots” in your vision
- You see sudden flashes of light
- You notice loss of any peripheral (side) vision
How are your eyes examined for flashes and/or floaters?
When an ophthalmologist examines your eyes, your pupils will be dilated with eye drops. During this examination, your ophthalmologist will carefully observe your retina and vitreous using a bright light. Evaluation for retinal tears usually requires a technique called scleral depression, for which your ophthalmologist will use an instrument to gently press on your eyelids. This office examination is done with minimal discomfort. Because your eyes have been dilated, you may need to make arrangements for someone to drive you home afterwards.
Floaters and flashes of light become more common as we grow older. While not all floaters and flashes are serious, you should always have a medical eye examination by an ophthalmologist to make sure there has been no damage to your retina.
What can be done about floaters?
Floaters can get in the way of clear vision, which may be quite annoying, especially if you are trying to read. Though most floaters will always be there, people usually notice less over time. Floaters can be surgically removed (with surgery called vitrectomy – Figure 3), but this is not performed routinely as most people have minimal symptoms after a couple of months. Even if you have had some floaters for years, you should have an eye examination immediately if you notice new ones.
What is retinal detachment?
The retina is the sensory tissue that lines the back wall of the eye. It can be described as the wallpaper of the back of your eye. A retinal detachment occurs when the retina is separated from the inside of your eye and can no longer transmit images properly through the optic nerve to the brain. The center of the retina is the macula. If the macula is involved in the detachment, the vision is often extremely blurred. If the macula is not involved in the area of detachment, there may be some loss of peripheral vision.
Is a retinal detachment serious?
Yes. A retinal detachment is a very serious problem that will almost always lead to blindness if not treated.
What causes retinal detachment?
As described above, in some cases vitreous separation can cause a tear (or tears) in the retina. As time passes, fluid from the center of the eye will pass through the tear and begin accumulating beneath the retina, causing a retinal detachment. There are some conditions that increase the likelihood of developing a retinal detachment. These include:
- Myopia (nearsightedness)
- Traumatic Injury
- A history of retinal detachment in either eye
- Family history of retinal detachment
What are the symptoms of retinal detachment?
- A new floater or several floaters can be hundreds) that appear suddenly
- Sudden flashes of light in the eye
- Seeing “cobwebs” or hairs in the field of vision
- Impression of a curtain or veil coming down over vision (loss of peripheral, and then central, vision)
- Blurred vision
- Pain is not a symptom of a detached retina
How is retinal detachment repaired?
A retinal detachment can be repaired in several different ways. The surgery chosen depends on the age of the patient, the type of retinal detachment, whether the patient has had cataract surgery or not, surgeon preference, and other factors. The four general categories of retinal detachment are:
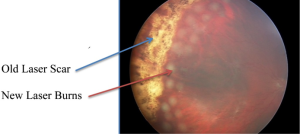
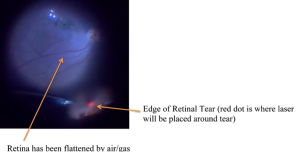
Figure 5
- Laser barricade (Figure 5) – does not fix the detachment but prevents it from spreading; can be done in the office).
- Pneumatic Retinopexy – a combination of treating the tear with cryotherapy (freezing treatment) or laser and the use of a gas bubble injected into the eye to help the eye get rid of the fluid. Figure 6 shows the injection of a gas bubble that will cover the tear in the retina. This prevents fluid from getting behind the retina and allows the body to absorb the fluid and flatten the retina.
- Scleral Buckle – a scleral buckle involves first treating the tear in the retina with cryotherapy (freezing treatment) and then placing a silicone band under the muscles around the eye to support the tear. The fluids can be drained from under the retina or a gas bubble can be injected into the eye similar to pneumatic retinopexy.
- Vitrectomy – vitrectomy involves the removal of the vitreous (floaters) from the eye using small instruments (Figure 3). This removes all the traction (pulling) on the retinal tear(s) and detachment. The vitreous space is then filled with a long-lasting gas bubble that keeps the retina flat until the tears heal. Laser is then used to seal the tear(s) (Figure 8).
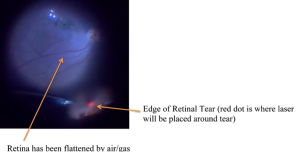
Figure 8
Sometimes both a scleral buckle procedure and a vitrectomy are used together to fix complex retinal detachments.
All diagrams from Ryan SJ, Retina. 4th ed. www.retinatext.com, Elsevier; 2006
See Your Eye Doctor Every Year
Why you should see an eye doctor annually
Your vision is a critical part of your overall health. When going in your regular annual physical checkup, it is important to also make sure that you have your vision checked as well. During an eye exam, your physician will check for signs of glaucoma, age-related macular degeneration, cataracts and diabetic retinopathy, among other diseases. So what is part of a traditional eye exam?
Eye Exam
The doctor will perform these typical eye tests as part of your annual exam. The first is the eye muscle movement test, which is meant to make sure that your eyes are aligning normally. Part of the test includes having your doctor ask you to track targets in various directions, then they will observe how your eye moves and note any areas of potential concern. If there are areas of concern, your doctor will prescribe treatments to deal with those concerns.
 Cover Test
Cover Test
The cover test is a check of how well your eyes are working in concert with each other. As you stare at a designated target in the distance, the doctor will cover and uncover your eyes one at a time. This will allow them to observe the movements of your eyes, watching to see if one of the eyes turns away from the target. This test can be repeated with the target close by as well.
External Test
During the external exam and pupillary reactions will test your pupils ‘reactions to both light and other objects at close distances. The doctor will also examine the exterior of the eye, looking for any changes in the condition of the white area of the eye and the overall position of the eyelids. If you continue to have a regular annual exam, then your doctor can track any changes over time and address them right away.
Visual Acuity Test
The visual acuity test requires you to sit in front of an eye chart, with letters that get gradually smaller as you read down the lines. You may be required to cover one eye or the other as part of this test. Depending on how good your vision is, you may be able to read the whole chart or be stuck part way down.
If you have difficulties with this chart, then you may be required to get a prescription for glasses or contacts to correct your vision issues. This will mean that you need to have a refraction test to determine your exact lens prescription. Additionally, you may need to have a glaucoma test to check the fluid pressure in your eyes falls within the normal range. The test is painless and usually takes just a few minutes to perform.
There are a few other tests that are included in a typical eye exam, but all these check the health of your eyes and their various parts. These tests are all geared to locating any potential issues with your eyes, but also how they can be indicative of other diseases or potential issues within your body as a whole. Be sure to have your eyes checked annually as part of an overall healthy lifestyle.
Macular Hole FAQs
What is Macular Hole?
A macular hole is a small full-thickness defect in macula, the most important region of your retina. The macula is the center of the retina, which is the light sensing part of the back of the eye. Formation of the hole causes loss of central vision (reading, driving, recognizing faces is affected).
What types of symptoms do patients with Macular Hole have?
Symptoms vary based on the size of the hole. The most typical symptoms are:
- Distortion of vision (called metamorphopsia) – letters look crooked
- Blurred vision or loss of visual acuity
- Dark spot at center of vision (central scotoma) – patients describe missing letters in words when looking right at the word. These dark spots are different than floaters as they do not move around.
- Patient often first notices the vision loss when they cover up the unaffected/good eye.
What causes a Macular Hole?
The most common cause of a macular hole is a posterior vitreous degeneration. This is when the vitreous gel that fills the center of the eye liquefies and separates from the back surface of the inside of the eye (the retina). This results in traction/pulling in the central macula. If there is enough traction a hole forms.
Direct ocular trauma by a blunt force, like a tennis ball, can cause macular holes to form as well. This group of patients is more likely to have spontaneous closure without surgery.
Who is at risk?
Most patients that develop macular problems are in their 60s or 70s and women are more commonly affected. Most people will experience vitreous degeneration, but macular hole is not very common. It is not associated with any systemic disease.
 How are they diagnosed?
How are they diagnosed?
The macula can be visualized during a routine eye exam after dilation of the pupil. Optical coherence tomography is a type of non-invasive imaging that allows your physician to view the macula and macular hole (if present) in cross-section. This allows your physician to measure the exact size of the hole and study the anatomy. This is useful for knowing the likelihood of closure with surgery.
How are they treated?
Small holes will often spontaneously close/heal without treatment. In some cases medication (Jetrea) can be injected into the eye that will release traction on the hole and allow it to close, however there are a very few eyes that are candidates for this medication. Most macular holes are treated with surgery.
Surgery consists of vitrectomy to remove the vitreous gel (floaters) from the middle of the eye (Figure 6). Micro-forceps are then used to gently peel the membrane from the retinal surface from around the hole (Figure 7).
What is the vision like after surgery?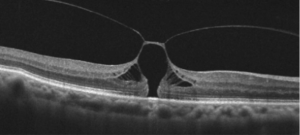
The vision is poor the day after surgery due to the gas bubble. Vision through gas is distorted and will remain so until the bubble resolves. There are usually position requirements after surgery to ensure the bubble is correctly positioned against the hole (each surgeon has their own post-operative position requirements based on their specific surgical technique). Historically, the patient was required to position face down for 14 days but currently close to 100% anatomical success can be achieved without face down positioning. The only requirement is that the patient not sleep on his/her back but to favor the opposite cheek being on the pillow.
Vision will improve after the gas bubble dissolves (this takes several weeks and timing depends on the type of gas used). Visual improvement can continue to occur for 9-12 months after successful surgery. If it has not already been removed, the cataract (cloudy lens of the eye) will worsen with this type of surgery, and this will cause worsening vision. Many times a combined approach is used and the cataract is removed at the same time as surgery for the macular hole.
Healing and approximation of the edges of the hole is out of the control of the surgeon. If the hole was small, the margins may come back perfectly and the vision returns to near normal. However, the tissues may not meet perfectly and there can be some residual distortion and blurred vision even if the hole is closed. There can be a persisting central dead spot in the vision if the central defect is filled in with scar tissue and the edges did not meet. This is most common in longstanding holes and larger holes.
 What are the restrictions after surgery? What are the risks of surgery?
What are the restrictions after surgery? What are the risks of surgery?
Restrictions in the postoperative period are most commonly related to the gas and the secondary poor vision. You cannot fly or travel to the mountains with an eye filled with gas. Patients should not drive or participate in activities that require depth perception and may result in injury.
Any intraocular surgery involving vitrectomy has a low risk of infection, bleeding, retinal detachment, and other complications, which can all lead to permanent vision loss. Risks, benefits, and alternatives to surgery should be discussed with your eye surgeon prior to proceeding with vitrectomy for macular hole.
Are e-readers bad for your eyes?
Are e-readers bad for your eyes?
Age Related Macular Degeneration
Age Related Macular Degeneration – Georgia Eye Institute
Age related Macular degeneration (AMD) is a leading cause of vision loss in those over 65. The associated anxiety of losing vision and independence can best be addressed with an understanding of the person at risk, the symptoms, and the treatments that improve the prognosis if the diagnosis is made early.
What is macular degeneration?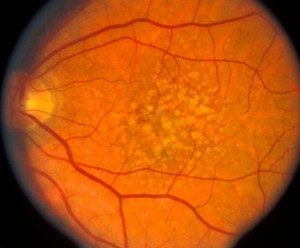
Macular degeneration is group of conditions that causes the central part of the retina, the macula, to lose the ability to see. This is an area behind the eye that cannot be easily seen or evaluated unless the eyes are dilated. There are two types of macular degeneration, wet and dry.
Dry macular degeneration is much more common and involves a slow process of aging cells that stop working and lead to blurred or missing areas in the central field of vision. It does not take away side vision.
Wet macular degeneration occurs when the aging retina grows new blood vessels that leak fluid and cause bleeding under the retina. These changes under the retina lead to sudden symptoms of blurred central vision and demand a prompt evaluation and treatment by an Optometrist.
It is much less common than dry AMD but receives more attention because of the potential for sudden severe loss of vision and because treatment is available. Patients are often ill prepared for the effect to lifestyle, hobbies, and work.
 Understanding the symptoms
Understanding the symptoms
Macular degeneration helps improve the prognosis, but it is very important to understand that early macular degeneration often has no symptoms. Therefore, nothing replaces regular dilated eye exams and the American Academy of Ophthalmology suggests an exam every one to two years after the age of 65.
Patients must remain vigilant by testing each eye alone for more advanced symptoms: blurred vision, distortion, or missing areas in the central vision. The patient may notice it is more difficult to see faces or read, but it is important to remember that with both eyes open, advancing macular degeneration in one eye can be missed.
One can avoid this by checking vision with one eye covered while reading the paper or doing a Sudoku puzzle. Symptoms such as bent/curved lines, or missing letters can be noticed with single corrective eye exam.
Monitoring your vision is good at all ages but from a practical standpoint we can use our personal risk factors to guide our frequency of monitoring for symptoms. While we recognize an increased risk in blue eyed Caucasians of northern European descent, there is three risk factors that demand greater attention: a positive family history, a history of past or present smoking, and advancing age. Every race has an increased risk with advancing age, but a family history can be the most predictive. Genetic testing is not recommended yet but patient with a positive family history of AMD requires earlier and more frequent exams to identify early disease and to allay unnecessary fears if the exam is normal.
While you can’t pick your genetics or stop aging, smoking is the most important risk factor that you can modify. If you are concerned about vision loss from AMD, you must stop smoking. After your dilated macular exam, you and your doctor can tailor a reasonable frequency for exams and home monitoring for advancing AMD.
If monitoring detects new distortion, blurred vision, or areas of missing vision, you should seek prompt consultation with your eye doctor. Early diagnosis is important because it improves prognosis. Diagnostic evaluations may be as simple as a dilated retinal exam with your doctor but could also include an optical coherence tomography (OCT).
This is a retinal scan that can detect small amounts of retinal fluid that may otherwise be missed. More advanced testing with a retina specialist may include an injection of a contrast agent into your arm to perform an angiogram of the retinal vessels to look for abnormal new vessels. These tests determine your potential need for treatment.
Treatment Options
Treatment of wet AMD has seen great strides over the past 10 years. The prognosis has greatly improved with the introduction of injectable medication. Patients who were once certain to become blind have a much better chance of maintaining useful vision.
The importance of early treatment is highlighted by the 90% of people who will maintain or have improved vision if injection treatment is started during early onset of the disease. Regular injections of Eylea, Lucentis, or off- label use of compounded Avastin suppresses leakage and bleeding but unfortunately does not cure the disease. While a few patients can stop therapy, most require regular monitoring and injections indefinitely.
There is no current treatment for dry macular degeneration, but research is looking for ways to stop the degenerative process. Most therapy is supportive in nature with low vision aids to help with reading and daily tasks. Low vision aids can also be of great help to patients with wet AMD.
Vitamin therapy is based on the Age Related Eye Disease Studies that evaluated the role of high dose vitamin therapy at reducing the incidence of AMD and vision loss. In the AREDS II trial, those patients taking the supplements with lutein/zeaxanthin had a 26% reduced risk of developing advanced AMD compared to those not taking the supplement. Most of the participants also took a multivitamin.
Macular degeneration is a complex topic that can cause anxiety because it is poorly understood, and we all fear the loss of vision and independence. With education, routine monitoring, and prompt therapy, the poor vision, and fear of AMD can be minimized.
We stress regular dilated eye exams, not smoking, and a diet in green leafy vegetables and AREDS II vitamin supplements to reduce its effect.

 She says that eye stress is all too common, in the form of…
She says that eye stress is all too common, in the form of…