Diabetic Retinopathy FAQs
What is diabetic retinopathy?
Long-standing diabetic disease (in Type I or Type II diabetics) can lead to changes in the back of the eye that can cause a decrease in vision. Specifically, high blood sugar causes damage to the small blood vessels in the retina (layer at the back of the eye that sense light). This damage leads to multiple changes to the retina, especially to the macula, which is responsible for central vision (Figure 1).
What are the different types?
There are two main types of diabetic retinopathy – “Non proliferative Diabetic Retinopathy” and “Proliferative Diabetic Retinopathy.” Proliferative indicates that new, abnormal blood vessels are growing inside the eye, which can lead to bleeding, retinal detachment, and high pressure (all leading to vision loss). Proliferative disease is more sever, but legal blindness can be caused by changes from non-proliferative disease.

Figure 1 – Normal Macula (the central part of the retina responsible for central vision)
Why do people lose vision from diabetic retinopathy?
Diabetes can lead to vision loss for many reasons, including:
- Swelling in the center part of the vision (Macular edema)
- Loss of blood flow to the center part of the vision (Macular ischemia)
- Bleeding into the central part of the eye (Vitreous hemorrhage)
- Detachment of the back layer of the eye from scar tissue (Retinal detachment)
How is it diagnosed?
The retina can be visualized during a routine eye exam after dilation of the pupil (Figure 3). Optical coherence tomography is a type of non-invasive imaging that allows your physician to view the macula and macular edema (if present) in cross-section (Figures 3 and 4). This is useful for following the disease over time.
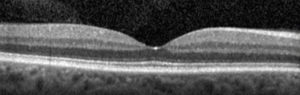
Cross sectional image (Optical Coherence Tomography, or OCT) of a normal macula. The “dip” in the center is the very center part of the vision, or the “fovea.” This is the “20/20? portion of the vision.
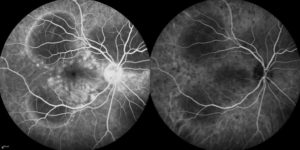
Figure 5. Photograph of the retina (angiogram) that shows loss of blood flow (dark areas).
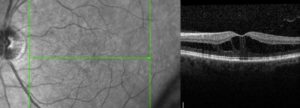
Figure 4. Cross sectional image (OCT) of a macula with diabetic macular edema. Notice the loss of the “dip” and black spaces in the retina. The retina is also thicker because of the swelling. This thickening leads to decreased vision.
How is it treated?
Treatment of diabetic retinopathy depends on the type of disease present. Good blood glucose and blood pressure control are essential in stabilizing disease.
Macular Edema
Edema that affects the center part of the vision is initially treated with medication that is injected into the eye (Figure 6). There are several medications available (Avastin, Lucentis, Eylea, Osurdex implant, steroid). For certain types of edema laser may be used. Laser can be used to destroy leaking blood vessels. A newer technology (micropulse laser) uses non-destructive energy to cause the macula to release factors that cause vessels to stop leaking.
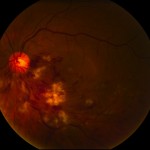
Figure 6. After the surface of the eye is anesthetized (numbed), a small amount of medication is injected into the middle of the eye (vitreous).
Proliferative Diabetic Retinopathy
Proliferative disease (especially if associated with bleeding [vitreous hemorrhage]) is generally treated with laser (panretinal photocoagulation). Laser is used to destroy sick tissue (areas in the back of the eye with loss of blood flow) – this causes abnormal blood vessels to shrink/resolve (Figure 7).
Vitreous Hemorrhage and Traction Retinal Detachment
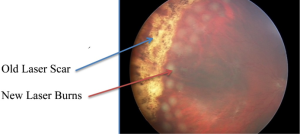
Figure 7. Photo of the retina shows vitreous hemorrhage covering the macula (center of vision) which blurs the vision. Laser scar can be seen peripheral to the blood. This patient required vitrectomy (surgery) to remove the blood.
Proliferative disease that is untreated will lead to bleeding and retinal detachment. The blood itself will usually not harm the eye and will often resolve spontaneously. If the blood does not resolve or if there is retinal detachment that treats the macula (center part of the vision), surgery (vitrectomy) is necessary,. This surgery is performed in an operating room. Small instruments are introduced through micro-cannulas. One instrument provides light and the other instruments to remove blood and scar tissue and place additional laser (Figure 8).
When should a diabetic have a complete eye exam?
A type I diabetic should have their eyes examined within 3-5 years after diagnosis and yearly thereafter if no eye disease is found. A type II diabetic should have their eyes examined at the time of diagnosis and yearly thereafter if no eye disease is found. If diabetic retinopathy is present, follow-up and treatment depends on the severity of the disease or any other issues you may have.

Removal of the vitreous from inside the eye using the “vitrector” (left side of picture). A small instrument (right side of picture) provides the light to see inside the eye. This is done under a microscope.
